In the labyrinth of modern healthcare, where every ailment has a protocol and every symptom a checklist, there lies a complex and often overlooked narrative: the treatment of chronic illness in women. As we delve into the intricate tapestry of medical history and contemporary practice, a question emerges from the shadows: Is there a bias in how chronic illnesses are treated in women? This inquiry invites us to explore beyond the confines of clinical diagnoses and into the realm of gender dynamics, societal norms, and medical assumptions. With a neutral lens, we embark on a journey to uncover the truths and myths surrounding this pressing issue, seeking to understand whether the medical world has inadvertently woven a gendered bias into its treatment of chronic ailments. As we peel back the layers, we aim to illuminate the experiences of countless women navigating the healthcare system, striving for clarity, equity, and ultimately, healing.
Gender Disparities in Medical Diagnosis and Treatment
In recent years, increasing attention has been directed towards the potential bias in the treatment of chronic illnesses among women. Despite advancements in medical science, studies reveal that women often experience longer wait times for diagnosis, are more likely to have their symptoms dismissed as psychological, and are underrepresented in clinical trials. This can lead to significant disparities in the care they receive. These discrepancies are particularly pronounced in conditions such as heart disease, autoimmune disorders, and chronic pain syndromes.
- Heart Disease: Women frequently receive delayed diagnoses compared to men, despite heart disease being a leading cause of death for women. Symptoms in women can differ from the classic signs often seen in men, leading to misdiagnosis.
- Autoimmune Disorders: Conditions like lupus and rheumatoid arthritis are more prevalent in women, yet research funding and clinical trials often do not reflect this gender disparity, resulting in treatments that are not always tailored to women’s needs.
- Chronic Pain: Women are more likely to be prescribed sedatives rather than pain medication, and their pain is often minimized or attributed to emotional factors, affecting their quality of life and treatment outcomes.
Addressing these issues requires a concerted effort to enhance gender-specific research, increase awareness among healthcare professionals, and ensure equitable treatment protocols that recognize the unique experiences of women with chronic illnesses. By fostering an inclusive medical community, we can work towards eliminating these biases and improving health outcomes for all patients.
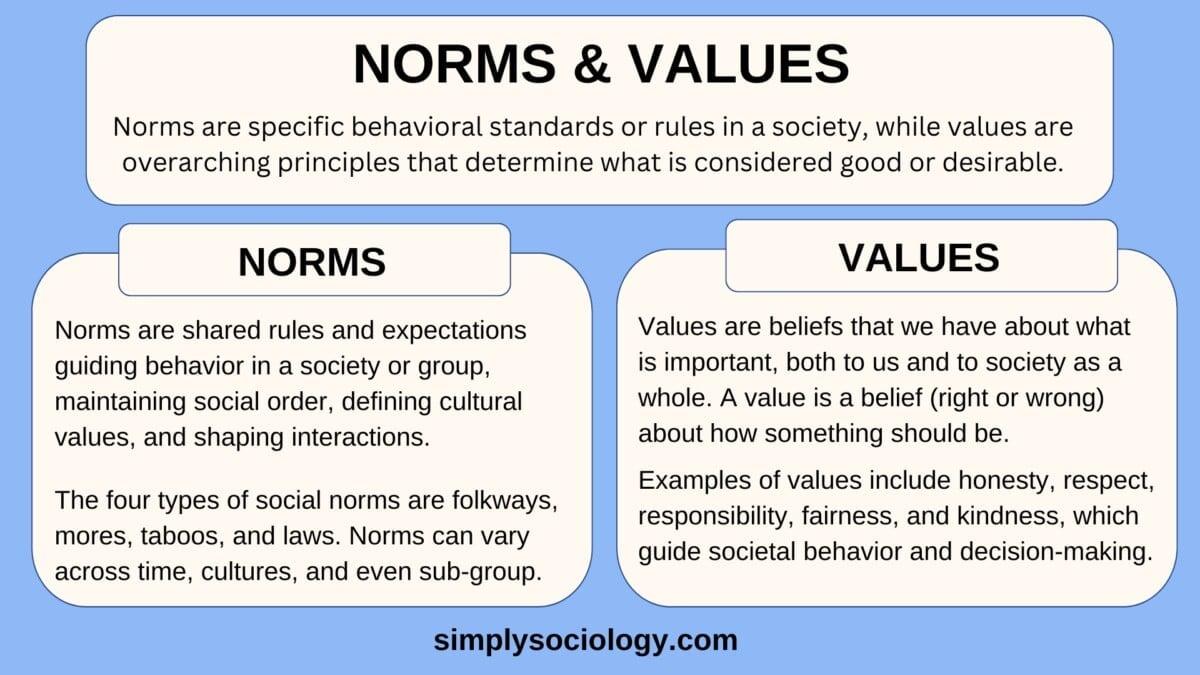
The Role of Societal Norms in Healthcare Bias
Societal norms, often unseen but deeply influential, can significantly impact healthcare delivery, particularly in the realm of chronic illness treatment for women. These norms shape perceptions about women’s health needs, influencing both the expectations and experiences of patients and providers. For instance, the traditional view that women are more emotional may lead to their symptoms being underestimated or misattributed to psychological factors rather than physical conditions. This can result in delays in diagnosis and inadequate treatment plans.
Moreover, healthcare systems may inadvertently perpetuate these biases through practices and policies that reflect historical gender roles. Consider the following ways societal norms manifest in healthcare settings:
- Gender Stereotyping: Women may be perceived as exaggerating pain, which can lead to their symptoms being taken less seriously compared to men.
- Resource Allocation: Research funding often prioritizes diseases more prevalent in men, leading to gaps in knowledge about conditions predominantly affecting women.
- Communication Barriers: The expectation for women to be nurturing and accommodating can hinder assertive communication about their health needs.
Addressing these biases requires a multifaceted approach, involving education, policy reform, and cultural shifts within the healthcare community to ensure equitable treatment for all patients.

Bridging the Gap: Strategies for Equitable Treatment
Addressing disparities in the treatment of chronic illnesses among women requires a multi-faceted approach, blending innovative healthcare strategies with a deep understanding of societal influences. Healthcare professionals must be trained to recognize and counteract their own biases, ensuring that diagnostic and treatment processes are based on objective criteria rather than preconceived notions. Patient-centered care should be prioritized, where women feel heard and their symptoms are taken seriously, leading to more accurate diagnoses and effective treatment plans.
Implementing community outreach programs can help educate women about their health rights and available resources, empowering them to advocate for themselves within the healthcare system. Collaboration between healthcare providers and policy-makers is essential to create regulations that mandate equitable treatment standards. Additionally, fostering a culture of inclusive research by prioritizing studies that focus on gender-specific manifestations of chronic illnesses will lead to more tailored and effective treatments. By embracing these strategies, the healthcare system can take meaningful steps towards achieving equity in chronic illness treatment for women.
Empowering Patients: Advocacy and Awareness in Chronic Illness Care
In the realm of chronic illness treatment, a subtle yet impactful bias often emerges, particularly affecting women. This bias can manifest in various forms, from the dismissal of symptoms to the underrepresentation in clinical trials. Women frequently report feeling unheard or having their symptoms attributed to psychological factors rather than physiological causes. This can lead to delays in diagnosis and treatment, ultimately affecting the quality of care they receive.
Key challenges faced by women include:
- Lack of representation in research studies, leading to treatments that may not be optimized for women’s unique biological needs.
- Societal stereotypes that may influence healthcare providers’ perceptions and decisions.
- Underdiagnosis and misdiagnosis due to atypical presentation of symptoms.
Addressing these biases requires a concerted effort in advocacy and awareness, empowering patients to demand equitable care and encouraging healthcare systems to adopt more inclusive practices. By highlighting these issues, we can foster a more balanced approach to chronic illness treatment that recognizes and values the diverse experiences of all patients.