In the labyrinth of modern healthcare, preventive care stands as a beacon of hope, promising to shield us from the ailments that lurk in the shadows of our futures. Yet, as we navigate this complex landscape, a curious conundrum emerges: the phenomenon of overdiagnosis. Imagine a world where our zealous pursuit of health inadvertently leads us into a maze of unnecessary treatments and unwarranted anxiety. Is overdiagnosis an unintended consequence of our preventive ambitions, or is it a necessary cautionary tale in the quest for early detection? This article delves into the nuanced world of overdiagnosis in preventive care, unraveling the threads of evidence and opinion that weave together this intricate tapestry of modern medicine. Join us as we explore whether our well-intentioned vigilance has, paradoxically, become a problem of its own.
Understanding Overdiagnosis in Preventive Medicine
In the realm of preventive medicine, overdiagnosis emerges as a multifaceted challenge that can undermine the very essence of early detection and intervention. Overdiagnosis occurs when individuals are diagnosed with conditions that, although identified through screening, would never have caused symptoms or death. This phenomenon can lead to unnecessary treatments, anxiety, and financial burdens. As healthcare systems strive to balance the benefits of early detection with the risks of overdiagnosis, it is crucial to consider several factors:
- Screening Sensitivity: Highly sensitive tests may detect abnormalities that are clinically insignificant, leading to overdiagnosis.
- Patient Awareness: Educating patients about the potential risks of overdiagnosis can empower them to make informed decisions regarding screenings.
- Medical Guidelines: Continuous evaluation and adaptation of screening guidelines can help mitigate the risk of overdiagnosis by focusing on high-risk populations.
In addressing overdiagnosis, healthcare professionals and policymakers must collaborate to refine screening protocols and prioritize patient-centered care. By fostering a deeper understanding of overdiagnosis, the healthcare community can work towards ensuring that preventive medicine achieves its primary goal: improving patient outcomes without causing harm.

The Fine Line Between Vigilance and Excess
In the realm of preventive care, striking a balance between necessary vigilance and the risk of overdiagnosis is an intricate dance. Healthcare providers are constantly navigating this fine line, where the goal is to identify potential health issues before they manifest into serious problems. However, the challenge arises when the pursuit of early detection leads to identifying conditions that may never cause symptoms or harm.
- Increased Anxiety: Patients may experience unnecessary stress and anxiety when faced with diagnoses that may never impact their quality of life.
- Financial Implications: Overdiagnosis can lead to excessive healthcare costs, both for the patient and the healthcare system.
- Unnecessary Treatments: Interventions for conditions that are unlikely to progress can expose patients to risks without clear benefits.
As we advance in medical technology and screening techniques, the healthcare community must continuously evaluate the implications of overdiagnosis, ensuring that the scales tip in favor of genuine health benefits rather than unnecessary medicalization.
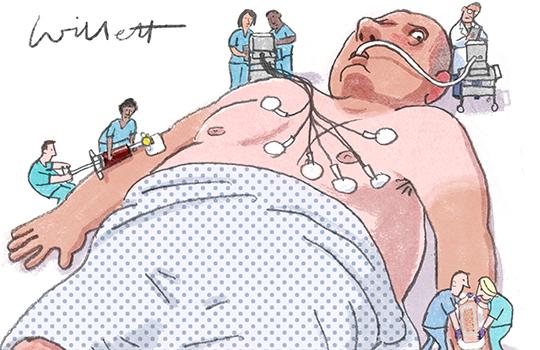
Impacts of Overdiagnosis on Patient Well-being
In the realm of preventive care, the phenomenon of overdiagnosis can have profound effects on a patient’s well-being. Emotional distress often accompanies a diagnosis, even when it turns out to be unnecessary. Patients may experience anxiety, depression, or a diminished quality of life due to the fear of a disease they may never actually suffer from. The psychological burden can be compounded by the stigma associated with certain conditions, leading to social isolation or altered self-perception.
- Unnecessary treatments: Patients may undergo invasive procedures, medication regimens, or lifestyle changes that are not required, leading to side effects or complications.
- Financial strain: The cost of additional tests, treatments, and follow-up care can be substantial, affecting not only the patient’s finances but also their family’s economic stability.
- Healthcare system burden: Overdiagnosis can strain healthcare resources, diverting attention and funds away from patients with genuine needs.
Addressing overdiagnosis requires a delicate balance between vigilance in early detection and the avoidance of unwarranted alarm, ensuring that preventive care truly benefits patient health without unnecessary harm.

Strategies for Reducing Unnecessary Diagnoses
In addressing the challenges of overdiagnosis in preventive care, healthcare professionals can adopt several strategies to ensure that diagnoses are both necessary and beneficial. Firstly, enhancing patient education is crucial. By informing patients about the potential risks and benefits of certain screenings and tests, they can make more informed decisions about their healthcare. This includes discussing the likelihood of false positives and the implications of overdiagnosis. Providing clear, accessible information empowers patients to participate actively in their care, potentially reducing the demand for unnecessary tests.
Another effective approach involves implementing evidence-based guidelines. By adhering to established protocols that prioritize high-value care, healthcare providers can minimize the occurrence of overdiagnosis. This might include:
- Regularly updating clinical guidelines based on the latest research.
- Incorporating decision support tools within electronic health records to assist clinicians in making informed choices.
- Encouraging a culture of shared decision-making, where clinicians and patients collaboratively discuss the necessity and potential outcomes of diagnostic procedures.
Additionally, fostering an environment where continuous professional development is encouraged can help clinicians stay informed about the nuances of overdiagnosis. By prioritizing these strategies, the healthcare system can move towards a more balanced approach in preventive care, ensuring that patients receive necessary and appropriate diagnoses.