In a world teeming with information, the line between fact and fiction often blurs, especially when it comes to topics as essential yet misunderstood as contraceptives. Myths swirl around like autumn leaves caught in a gust, persistent and colorful, yet detached from the roots of truth. From whispered rumors in school hallways to sensationalized headlines, misconceptions about contraceptives have woven themselves into the fabric of societal discourse, influencing decisions and shaping perceptions. This article embarks on a journey to unravel these myths, shedding light on the realities of contraceptive use. By debunking these common misconceptions, we aim to empower individuals with knowledge, enabling informed choices about their reproductive health. Join us as we separate myth from reality and illuminate the path to understanding in the realm of contraceptives.
Understanding Hormonal Contraceptives and Weight Gain
One of the most prevalent myths surrounding hormonal contraceptives is their supposed link to significant weight gain. It’s a topic that often comes up in conversations, leading to hesitation or fear of using these birth control methods. However, it’s essential to separate fact from fiction. While some individuals may experience minor fluctuations in weight when starting hormonal contraceptives, research has not consistently supported the idea that these methods lead to substantial weight gain. Studies have shown that any changes are typically temporary and can be attributed to water retention or other factors, rather than an actual increase in body fat.
- Understanding the Science: Hormonal contraceptives like the pill, patch, or injection can cause changes in appetite or fluid retention, but these effects are generally mild and short-lived.
- Individual Responses Vary: It’s important to remember that everyone reacts differently. What one person experiences might not be the same for another, emphasizing the need for personalized medical advice.
- Healthy Lifestyle Choices Matter: Maintaining a balanced diet and regular exercise routine can help mitigate any potential weight-related side effects.
Ultimately, the fear of weight gain should not overshadow the myriad benefits that hormonal contraceptives offer, from preventing pregnancy to regulating menstrual cycles and alleviating acne. As always, consulting with a healthcare professional can provide clarity and reassurance tailored to your individual health needs.
Decoding the Myth of Infertility and Long-term Use
One prevalent misconception is that using contraceptives over an extended period can lead to infertility. This myth often causes unnecessary worry and hesitation among individuals seeking reliable birth control options. In reality, most contraceptive methods, whether hormonal or non-hormonal, do not have a long-term impact on fertility. When you decide to stop using these methods, your fertility typically returns to its normal state.
- Hormonal contraceptives: These may cause a temporary delay in the return of fertility, but this is usually short-lived. Studies show that after discontinuing use, individuals generally regain their ability to conceive within a few months.
- Intrauterine devices (IUDs): Whether hormonal or copper-based, IUDs are designed to be reversible. Fertility is usually restored immediately after removal.
- Barrier methods: These include condoms and diaphragms, which have no impact on long-term fertility as they work by preventing sperm from reaching the egg.
Understanding these facts can empower individuals to make informed choices about their reproductive health without the shadow of unfounded fears.

The Truth About Birth Control and Cancer Risks
When discussing contraceptives, a common concern that arises is the potential link between birth control and cancer risks. However, much of the information circulating on this topic is rooted in misconceptions. Scientific studies have shown that while there are certain risks associated with hormonal contraceptives, the benefits often outweigh these concerns for many individuals. Here’s a closer look at the facts:
- Breast Cancer: Some studies suggest a slight increase in the risk of breast cancer for current and recent users of hormonal birth control. However, this risk diminishes over time after discontinuing use.
- Ovarian and Endometrial Cancer: Contrary to popular belief, hormonal contraceptives can actually reduce the risk of ovarian and endometrial cancers. This protective effect increases with longer use and can last for years after stopping the pills.
- Cervical Cancer: Long-term use of hormonal contraceptives may be associated with a higher risk of cervical cancer, but regular screenings and HPV vaccinations can mitigate this risk significantly.
It’s crucial to weigh these considerations with the guidance of a healthcare professional to determine the best approach for your personal health needs. While the conversation around contraceptives and cancer is complex, informed choices are the key to navigating these waters effectively.
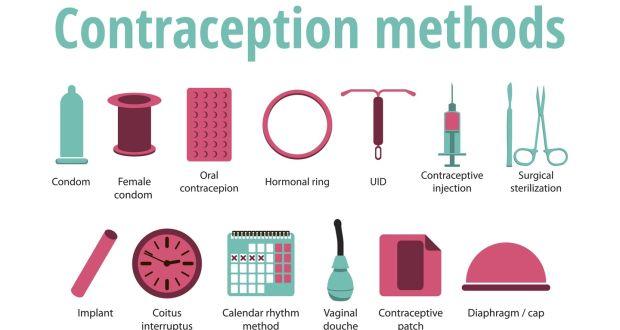
Navigating Contraceptive Options: Expert Advice for Informed Choices
- Myth: Contraceptives Cause Infertility – A common misconception is that using contraceptives can lead to permanent infertility. In reality, most contraceptive methods are designed to be reversible, allowing individuals to resume their natural fertility after discontinuation. Whether it’s hormonal pills, IUDs, or implants, scientific studies have consistently shown that fertility levels return to normal within a few months after stopping use.
- Myth: Birth Control Pills Protect Against STIs – While oral contraceptives are highly effective at preventing pregnancy, they offer no protection against sexually transmitted infections (STIs). For STI prevention, using condoms in conjunction with other contraceptive methods is recommended. This dual approach provides both reliable pregnancy prevention and a barrier against infections.
- Myth: Emergency Contraception Is Abortion – Emergency contraception, often referred to as the “morning-after pill,” is frequently misunderstood. It works primarily by delaying ovulation and does not terminate an existing pregnancy. Thus, it is not an abortifacient. Understanding this distinction is crucial for making informed decisions in time-sensitive situations.