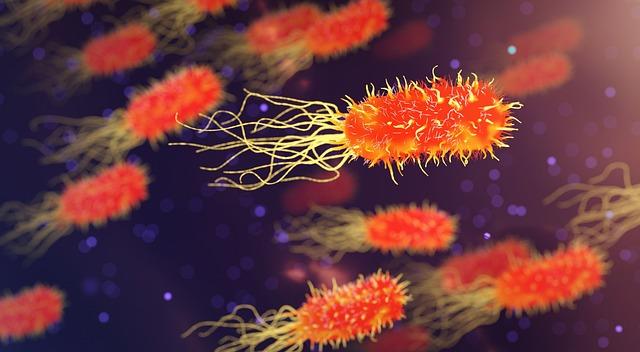
In the intricate tapestry of human health, few threads are as complex and revealing as those woven by our genetic makeup. Among the myriad conditions influenced by our genes, diabetes stands out as a particularly enigmatic puzzle. While lifestyle choices and environmental factors are often highlighted in discussions about diabetes, the silent orchestration of our genes plays a crucial, albeit less visible, role in determining our susceptibility to this condition. As science delves deeper into the genome, a clearer picture emerges, illuminating how our genetic inheritance shapes our risk of developing diabetes. This article embarks on a journey through the genetic underpinnings of diabetes, exploring how tiny variations in our DNA can have profound implications for our health. By understanding the genetic factors at play, we move closer to personalized prevention strategies and treatments, offering hope for a future where diabetes risk is not merely a roll of the dice, but a narrative we can begin to rewrite.
Unlocking the Genetic Code: How Your DNA Influences Diabetes Risk
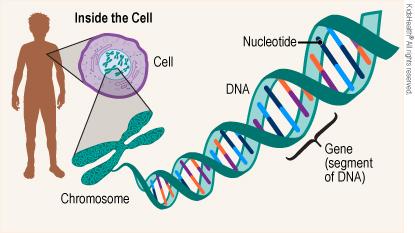
Our DNA is like a roadmap, guiding the intricate pathways of our health. When it comes to diabetes, genetic factors can play a significant role in determining an individual’s risk. While lifestyle choices such as diet and exercise are pivotal, the genetic component is an unavoidable part of the equation. Genetic predispositions can influence how our bodies respond to insulin, how effectively glucose is processed, and even how our body stores fat. Researchers have identified several genes associated with an increased risk of developing both type 1 and type 2 diabetes. These discoveries not only enhance our understanding of the disease but also open doors for personalized medical approaches.
- Family History: A strong indicator, as diabetes can run in families.
- Gene Variants: Certain variations in genes, such as those affecting insulin production, can elevate risk.
- Ethnic Background: Some ethnic groups are genetically predisposed to higher rates of diabetes.
Understanding these genetic influences allows for more effective prevention strategies. By combining genetic insights with lifestyle modifications, individuals at risk can better manage their health. As science progresses, the potential for genetic testing to become a routine part of diabetes risk assessment grows, promising a future where prevention is tailored to one’s unique genetic makeup.
Exploring Genetic Markers: Identifying Key Players in Diabetes Development
As we delve into the fascinating world of genetics, it becomes clear that certain genetic markers play a pivotal role in the development of diabetes. These markers, or specific sequences of DNA, can significantly influence an individual’s predisposition to the disease. Understanding these markers is akin to deciphering a complex biological code that holds the secrets to why some people are more susceptible to diabetes than others. Research has identified several key genetic markers associated with both Type 1 and Type 2 diabetes, which are crucial for unraveling the intricate web of genetic and environmental interactions.
- HLA Genes: Particularly linked to Type 1 diabetes, these genes are involved in immune system regulation. Variations can trigger an autoimmune response that attacks insulin-producing cells.
- TCF7L2 Gene: Often associated with Type 2 diabetes, this gene affects insulin secretion and glucose production, playing a significant role in how the body metabolizes sugar.
- SLC30A8 Gene: This gene influences the function of beta cells in the pancreas, impacting insulin release and overall glucose homeostasis.
- PPARG Gene: Known for its role in fat cell differentiation, this gene affects insulin sensitivity and is a notable factor in the development of Type 2 diabetes.
Exploring these genetic markers not only enhances our understanding of diabetes risk but also paves the way for personalized medicine approaches, enabling tailored prevention strategies and treatments that consider an individual’s unique genetic makeup.
Bridging Genes and Lifestyle: Personalized Strategies for Diabetes Prevention
In the intricate dance between our genetic makeup and lifestyle choices, understanding how genes influence diabetes risk is crucial. Our DNA contains numerous genes that can predispose us to various health conditions, including diabetes. However, possessing certain genetic markers does not seal one’s fate. Instead, it offers a roadmap to tailor lifestyle strategies that can significantly mitigate risk. Genetic predisposition can affect how our bodies process sugar, insulin sensitivity, and even appetite regulation. Recognizing these nuances allows individuals to adopt more informed, personalized lifestyle changes.
Consider the following strategies for bridging genes and lifestyle in diabetes prevention:
- Dietary Adjustments: Opt for a diet rich in whole foods and low in processed sugars. This not only helps in managing weight but also in stabilizing blood sugar levels.
- Regular Physical Activity: Engage in exercises that enhance insulin sensitivity and promote cardiovascular health. Tailor your routine to what suits your body best.
- Stress Management: Implement mindfulness techniques such as meditation and yoga, which can help regulate hormones and reduce the risk of diabetes-related complications.
- Regular Monitoring: Stay proactive with regular health check-ups to monitor glucose levels and adjust lifestyle strategies as needed.
By intertwining genetic insights with these proactive lifestyle choices, we pave the way for a healthier future, potentially reducing the onset of diabetes even for those with a genetic predisposition.

From Research to Reality: Implementing Genetic Insights in Diabetes Management
The intricate dance of genetics plays a crucial role in determining an individual’s predisposition to diabetes. Advances in genetic research have unveiled specific gene variants that significantly influence one’s likelihood of developing this chronic condition. By examining these genetic markers, scientists can now predict potential risks and tailor preventive measures accordingly. This personalized approach not only enhances early detection but also paves the way for more effective management strategies, transforming the landscape of diabetes care.
- Personalized Treatment Plans: Genetic insights allow healthcare providers to customize treatment plans that align with an individual’s unique genetic makeup.
- Early Risk Identification: By identifying genetic markers early, interventions can be implemented before the onset of symptoms, potentially delaying or preventing the disease.
- Enhanced Understanding: Understanding the genetic underpinnings of diabetes fosters a deeper comprehension of the disease, leading to innovative research and therapies.
Incorporating genetic insights into diabetes management marks a significant shift from a one-size-fits-all model to a more nuanced, individualized approach. This evolution not only empowers patients but also enhances the precision and efficacy of medical interventions, offering new hope in the battle against diabetes.